INTRODUCTION
Every so often, we have a patient who presents with clinical challenges that need to be handled outside of the usual protocol. So it was with Lucinda, who presented with caries in 2 specific teeth that would normally have been treated by doing extractions. However, the health history showed Fosamax use and, upon further questioning, it was found that she had a history of heavy use of this prescription drug within the last 5 years. Consulting with Dr. Mark Ericson, our oral surgeon, the decision was madenot to remove teeth Nos. 3 and 18 because of potential healing problems in the bony socket sites due to the use of Fosamax.
This article will present the case introduced above, demonstrating the alternative treatment that was done, and the current research for deciding upon the course of action outlined below.
Fosamax Issues
Patients who have resorptive bone diseases such as osteoporosis (often women) can benefit from the use of oral bisphosphonates (BPs). For the last 11 years, a number of studies have been published that have documented the condition of osteonecrosis of the jaw (ONJ) that is associated with the use of oral BPs; thus called bisphosphonate-related osteonecrosis of the jaw, or BRONJ. From the studies, one can learn how these jaw necroses are tied to the use of BPs (such as Fosamax, risedronate, or alendronate).1
A clinical study important to the dental profession2 documented the healing issue faced when extracting teeth or bone work, namely slow or nonhealing of sockets. When patients have taken BPs for the treatment of osteoporosis, the ability for bone to heal after surgery can be limited. Should nonhealing take place, the patient’s life is affected, which can be a significant issue for the clinician too. The study observed 7 patients who had taken BPs and had extractions, with 6 of the patients having had sequestration during nearly a year of observation, and only 3 had experienced healing. It should be noted that the current standard treatment for BRONJ does not always provide good results.3
BPs have been widely, efficiently, and safely used for the treatment of osteoporosis, malignant hypercalcemia, bone metastasis of solid cancers, and multiple myeloma bone diseases. Accumulating recent reports describe that dental surgery treatments in patients with cancer or osteoporosis who have been receiving intravenous or oral BPs are associated with BRONJ.4
 |
 |
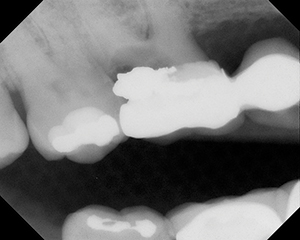
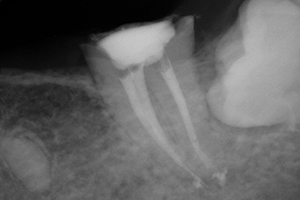
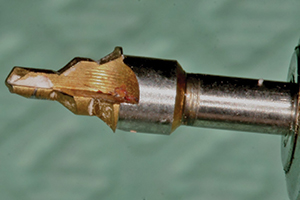
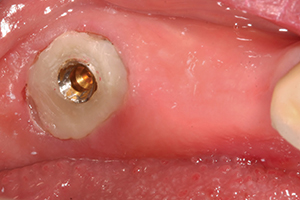
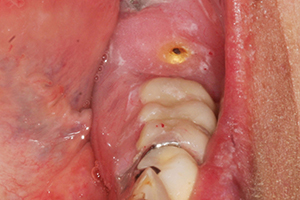
| Figure 1. Severe decay in tooth No. 3 that would usually require extraction. | Figure 2. Severe decay in tooth No. 18 that would usually require extraction. |
 |
 |
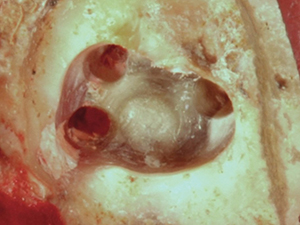
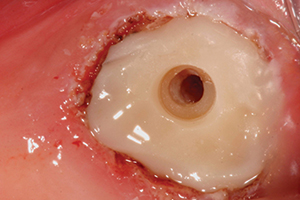
| Figure 3. Preserved root sealed with glass ionomers (GC Fuji II [GC America]). | Figure 4. Acytel resin unilateral partial over preserved root (tooth No. 3). Note: photo was taken after 4 months of wearing the prosthesis. |
 |
 |
| Figure 5. Tooth No. 18 root preserved with root canal and glass ionomer. | Figure 6. Retention preparation in No. 18 before composite resin was placed. |
Because BPs can be given to many cancer patients who also have a need for invasive dental care involving bone, it should be noted that ONJ cannot be effectively treated with debridement and antibiotics or even hyperbaric oxygen exposure. To prevent negative outcomes, the clinician must recognize that there are no effective treatments for ONJ. If treatment (such as extraction) is absolutely needed with a patient taking a BP, the treating medical doctor should be contacted about his or her BP delivery.5
A study concerning implant placement for those who were actively taking BPs showed no discernable healing issues. There was no significant difference between groups in the success rates of dental implants at stage-2 surgery (test 93.5%, control 95.5%).6 In another study, new bone formation in extraction sockets, bone area around the implant site, and bone-implant contact were not delayed in the bisphosphonate group.7
One report8 confirmed 2 other patients who experienced osteonecrosis from BP causes were successfully treated with teriparatide, when used as adjunct therapy in ONJ; this is because it has an anabolic effect and presumed role in accelerating bone healing. ONJ is a serious but infrequent condition that has been recently associated with nitrogen-containing bisphosphonate therapy. Teriparatide may be a useful adjunctive therapy when ONJ develops.
Hsiao et al9 found that the results of this preliminary short-term study suggest that patients taking long-term oral BPs can expect a satisfactory outcome with evidence of periradicular healing after conventional root canal treatment. Thus, root canal treatment may be considered a safe and realistic alternative to extraction in patients on bisphosphonate therapy.
The issue facing all dental clinicians is to extract or not to extract a tooth when the patient has been or is taking BPs. Even if the potential for osteonecrosis is small for any given patient, no dentist wants to be responsible for the patient getting this condition, and therefore, hesitancy on the decision to proceed with an extraction would be reasonable.
CASE REPORT
Lucinda presented as a new patient with extensive decay in 2 teeth that would have ordinarily been treated with extractions (Figures 1 and 2).
However, since her medical history included the use of Fosamax during a period of 5 years, it became apparent that extraction could lead to osteonecrosis in one or both sites, even though she reported having stopped taking the drug just prior to this dental visit. The question of an alternative approach seemed vital to getting an outcome that would provide a clinically good result while keeping her healthy.
 |
 |
| Figure 7. Glass ionomer in No. 18 prepared for ZAAG (ZEST Anchors) female attachment. | Figure 8. ZAAG One-Step Drill (ZEST Anchors) for ZAAG female attachment preparation. |
 |
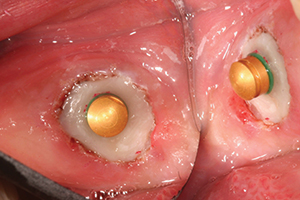 |
| Figure 9. ZAAG attachment cemented into tooth No. 18. | Figure 10. ZAAG male attachment placed into female ready for pickup. |
 |
 |
| Figure 11. Triad VLC Bonding Agent (DENTSPLY Trubyte) placed on lower partial denture for male ZAAG attachment. |
Figure 12. Triad DuaLine dual-cure (self- and light-cured) reline composite material (DENTSPLY Trubyte). |
 |
| Figure 13. Lower partial denture with the male ZAAG attachment snapped into female in tooth No. 18. |
The first course of action was to sever the maxillary bridge at crown No. 5 and to remove the existing crown on No. 3. After determining that the root canals of tooth No. 3 were calcified, the root was sealed with a glass ionomer (GC Fuji II [GC America]) (Figure 3). Since this tooth was without symptoms or swelling, it was determined that the roots could be left at this point. If any symptomology would appear at a later time, that could be dealt with by prescribing antibiotics. (Note: that need has not arisen, as of the writing this article.)
In order to restore the missing teeth, a unilateral partial denture of acytel resin was produced (Figure 4). At this point, this tactic has been successful for the patient.
Endodontic therapy was done on the lower left second molar (tooth No. 18) by Dr. June Chang to keep it from extraction (Figure 5). Since the patient would now need a removable partial denture, a unilateral type was offered with tooth No. 18 receiving a ZAAG attachment (ZEST Anchors) for distal-end anchorage. Because No. 18 had a temporary restoration after the root canal, because the occlusal height above to No. 15 was limited due to super eruption, and because crown lengthening was ruled out due to the BP issue; the tooth was restored with composite down into the pulp chamber. The preparation can be seen in Figure 6. This restoration allowed for preparation for the ZAAG female attachment placement (Figure 7) using the ZAAG drill (Figure 8) and the actual attachment.
The ZAAG female attachment was cemented into the preparation (Figure 9) using SEcure Cement (Parkell). The male attachment was tried in to evaluate the fit (Figure 10). The unilateral partial denture was primed with Triad VLC Bonding Agent (DENTSPLY Trubyte) (Figure 11), so that the male ZAAG could be “picked up” with Triad DuaLine (DENTSPLY Trubyte) dual-cure reline material (Figure 12). The result was giving the patient a firmly fitting unilateral partial denture, using a tooth that normally would have been extracted. Figure 13 shows the unilateral partial denture with the ZAAG attachment bonded in using Triad DuaLine.
CLOSING COMMENTS
During a dental career, we are sometimes presented with opportunities to be creative, offering the chance for a better outcome for a patient than his or her condition might normally warrant. Having written extensively about and practiced minimally invasive dentistry, this case where the patient presented with a history of BP use for treating osteoporosis required that kind of approach. This compromised situation and the research supporting caution led to the alternate treatment shown. Each subject tooth continues to function well under the partial dentures.
 ایران دنتال نیوز پایگاه مقالات و اخبار دندانپزشکی
ایران دنتال نیوز پایگاه مقالات و اخبار دندانپزشکی

